Vagus Nerve - Body Over Mind
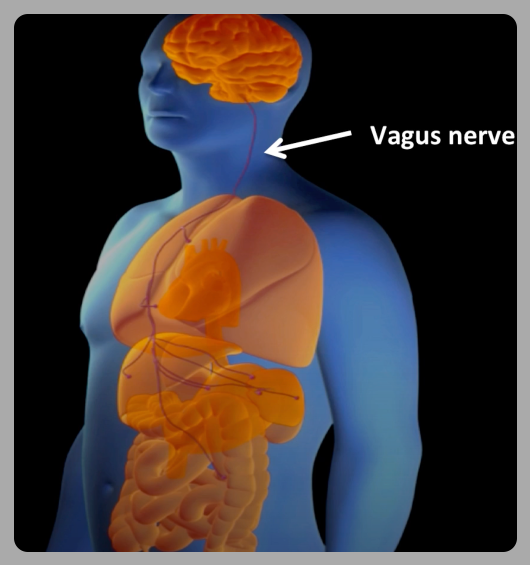
The vagus nerve is the longest cranial nerve, extending from the brainstem to the colon. It connects the mind with the body, functioning as a two-way communication highway. It is part of the “autonomous” nervous system.
The vagus nerve is the longest cranial nerve, extending from the brainstem to the colon. It connects the mind with the body, functioning as a two-way communication highway. It is part of the “autonomous” nervous system.
Surprisingly, 80% of the signals transmitted by the vagus nerve are from the body to the brain, with only 20% going from the brain to the body. Your body constantly ‘teaches’ your brain about internal states.
Deep belly breaths are a simple way to activate the vagus nerve. The body signals the brain to relax. It's the most straightforward life hack to get a quick micro-boost of well-being. You can do it anytime.
HRV training increases vagal tone measurably within 4-6 weeks, with improvements correlating to reduced inflammation markers (IL-6, TNF-α) and enhanced cognitive flexibility, as observed in neuroimaging studies.
Elite athletes and Navy SEALs utilize HRV biofeedback devices that measure heart rate variations. Breathing at five breaths per minute (coherent breathing) syncs heart rate with breath, creating ‘coherence’—a state where heart, mind, and emotions align—training the vagus nerve with real-time feedback.
Vagal tone, measured by heart rate variability, is associated with emotional regulation, immune health, and longevity. Each 10-ms increase in HRV is linked to approximately a 9% lower mortality risk.
Cold showers activate the vagus nerve and slow the heart rate. Regular cold exposure creates ‘hormetic stress,’ which functions as a form of strength and resilience training for the nervous system. Cold increases norepinephrine by 200-300% and trains vagal brake mechanisms, enhancing alertness and calm recovery. Wim Hof’s ice bath protocols are vagal training.
Chanting stimulates the vagus nerve through vibrations in the throat and chest. The 'Om' sound, when vocalized properly, produces specific frequencies (~136 Hz) that resonate through vagal pathways. Gargling, singing, and laughing activate similar neural circuits, which explains their calming effects and why laughter is considered a form of medicine.
Your gut has 500 million neurons linked to your brain through the vagus nerve. Mindful eating, slow chewing, or gentle abdominal massage train this ‘second brain.’ Fermented foods not only feed gut bacteria but also produce GABA and neurotransmitters that reach your brain via vagal pathways, explaining gut health’s impact on mood and anxiety.
Chronic stress shrinks vagal pathways via inflammation, but this damage is reversible. Meditation practitioners have thicker vagal fibers and more gray matter in regions that control emotions, with these changes becoming visible after 8 weeks of practice.
Stimulating the vagus nerve can increase the release of acetylcholine, which helps calm inflammation. Vagal tone is also closely associated with levels of hormones like oxytocin.
The vagus nerve exemplifies the power of biofeedback, where intentional physical actions can drive mental states. Vagal stimulation has been used as a treatment for epilepsy and depression. The benefits of yoga are also, at least in part, via the role of the vagus nerve.
Stephen Porges, a neuroscientist, was studying heart rate patterns in premature infants when he noticed that heart rate variability patterns predicted their survival rates better than traditional medical indicators. His 'Polyvagal Theory' identifies three distinct nervous system states: social engagement, fight-or-flight, and shutdown, each controlled by different vagal circuits.
“The vagus nerve is the great wanderer, connecting our hearts and minds in ways that make us uniquely human in our capacity for compassion and connection."
Porges' work transformed trauma therapy, showing that healing requires activating the social engagement system through safety cues rather than just processing traumatic memories.
Insights from Dr. Porges about the pivotal role of safety and socialization and the connection between them:
"Safety is not the absence of threat, it is the presence of connection...Safety is the treatment, and feeling safe is the goal...We need to feel safe to be social, and we need to be social to feel safe."
Kevin Tracey, an immunologist and neurosurgeon, discovered the 'inflammatory reflex’. Tracey found that stimulating the vagus nerve in mice prevented them from dying of overwhelming inflammation. The nervous system and immune system are integrated through vagal pathways. His team developed vagus nerve stimulation devices now used to treat rheumatoid arthritis and Crohn's disease.
“The vagus nerve is the body's natural anti-inflammatory pathway—evolution's solution to preventing our immune system from destroying us."

Deb Dana, a clinical social worker, translated polyvagal theory into practical therapy. While working with a client who felt ‘dead inside’ after trauma, she realized traditional talk therapy wasn’t reaching deeper neurobiological patterns. Using Porges’ work, she began helping clients identify their nervous system state—fight-or-flight, shutdown, or social engagement—before processing emotions or memories. Recognizing and naming their autonomic state enabled clients to shift consciously toward safety and connection.
“The autonomic nervous system is the foundation upon which our lived experience is built."
Polyvagal Theory, developed by Dr. Stephen Porges, explains how our autonomic nervous system responds to safety and danger through the vagus nerve. The theory identifies three main neural circuits:
- The Social Engagement System (Ventral Vagal) is associated with feelings of safety and connection. When this system is active, we can engage socially, think clearly, and feel calm. Our heart rate is regulated, we can make eye contact, and our voice has natural prosody.
- The Sympathetic System triggers when we perceive danger. It increases heart rate, releases stress hormones, and prepares the body for action.
- The Dorsal Vagal System activates when we perceive life-threatening danger with no escape. It causes immobilization responses, such as freezing, dissociation, or shutdown. Chronic activation can lead to depression, numbness, or disconnection.
The Polyvagal Theory has practical applications in therapy, education, healthcare, and personal development, helping to explain why trauma survivors may struggle with relationships or why someone might shut down during conflict. The theory emphasizes that feeling safe is fundamental to healing and growth. Therapists help patients identify which of the three circuits is activated and then suggest practices to guide them back to a calm, connected state.
The vagus nerve is the physical connection through which the body can regulate the mind in ways that enhance our emotional well-being.
